Anyone working in mental health care will agree that no patient with mental health problems is ever as simple as the “case studies” would have you believe. Comorbidity is the norm. Much of that comorbidity, in adults at least but often also in teenagers, is related to drug and alcohol use – something that may easily have developed in an effort to self-manage the underlying mental health problems.
I’m sure we all know people whose underlying mental health diagnoses were missed because of substance use and whose lives were shattered as a result. The person who comes to mind for me is a clever and engaging elderly woman whose severe bipolar disorder was missed for more than three decades because of concomitant alcoholism, and whose career and relationships with family (including her children) all fell apart as a result. She was diagnosed and treated just in time to avoid homelessness.
It is important not to get blinded to other possibilities by preoccupation with the substance use but in people presenting with this sort of complexity the issue is often “Where do I start?” The burning question is “How much of this person’s suffering is being caused by the substances they consume and will things get better when the person stops using them or is what I see related to the underlying condition?”
The situation can be overwhelming even for experienced practitioners.
Guidelines
The Matilda Centre for Research into Mental Health and Substance Use at the University of Sydney is dedicated to “increasing the knowledge base around the effective prevention and treatment of mental and substance use disorders.” Late last year the Matilda Centre published the 2nd edition of their Guidelines on the management of co-occurring alcohol and other drug and mental conditions in alcohol and other drug treatment settings (referred to as the Comorbidity Guidelines) and launched a website to help disseminate them. From that dedicated website you can read and download the guidelines or order a hard copy.
Education
As a bonus the Comorbidity Guidelines website also offers recordings of a series of amazing webinars on subjects ranging from Motivational Interviewing to managing comorbidity in the context of a whole range of mental health conditions from anxiety and depression to trauma and personality disorder and more.
There are also 12 online modules which make up a training program suitable for anyone working with people experiencing mental health difficulties in the context of drug and alcohol use. These modules clarify the guidelines and reinforce the information in them.
Online tools
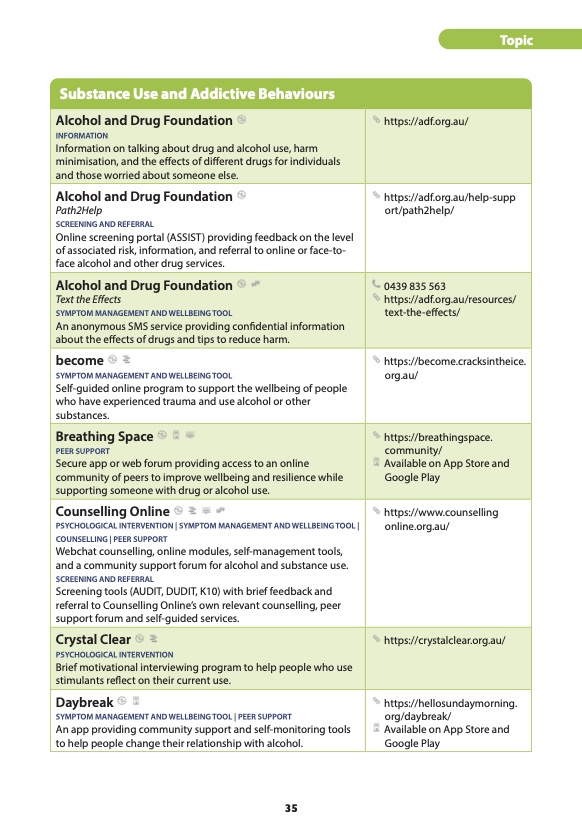
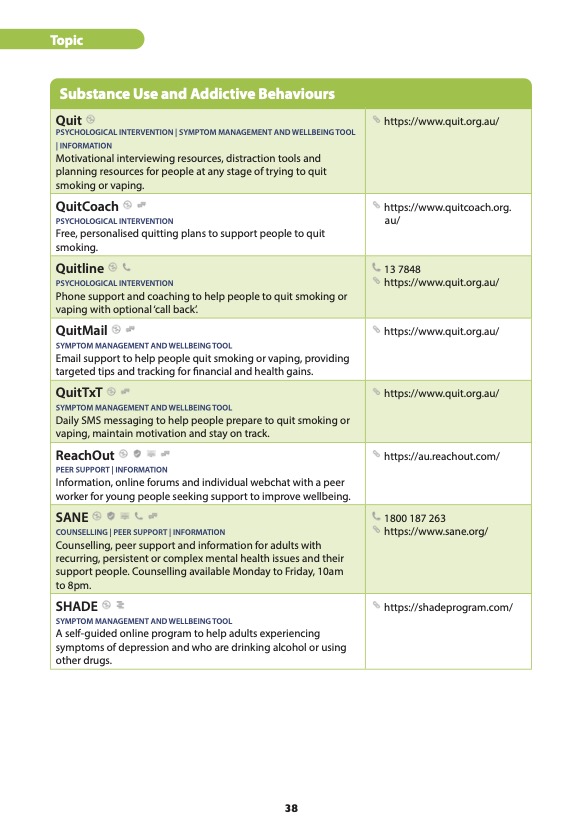
Digital resources to help us care for these patients and clients are unfortunately not as common as we would like. The eMHPrac Health Practitioner Guide to Digital Mental Health Services and Resources which confines itself to Australian developed evidence based digital resources provides a list of tools which may be of use to practitioners in these circumstances. Worth a special mention is the aptly names Hello Sunday Morning website, dedicated to helping people change their relationship with alcohol. That site provides access to validates assessment tools, information about alcohol and personal stories. Also available from the site (or from wherever else you usually get your apps) is the Daybreak app which provides users with self-monitoring tools and support from a like-minded community. The app is available free of charge.
For people with complex needs its also worth remembering Sane Australia’s peer support chat groups and forums. If tackling problems that are complex and entrenched is overwhelming for the practitioner it is also overwhelming for the person trying to deal with them. Support from others who have experienced similar problems can make a big difference.



Psychiatric Support for GPs
Phone-based psychiatric support to help GPs help people with complex needs is also available 7.00am to 7.00pm Monday to Friday through GP Psych Support. GPs (but only GPs) can call the line and speak to a psychiatrist with or without the patient in attendance. GPs need to register on the website to use the service. If the GPs you work with are unaware of the service, they might be grateful for some information about it, especially if it is difficult to see a psychiatrist in your area.
Importantly, GP Psych Support is publicly funded and free of charge to all GPs registered with the service.